Macrophage Tamers.
How does the Translational Cellular and Molecular Biomedicine Laboratory Work?
Can the immune system be reprogrammed and how will this help defeat cancer and myocardial infarction? How to prevent implants from being rejected by the body? Why can large projects be implemented only in cooperation?
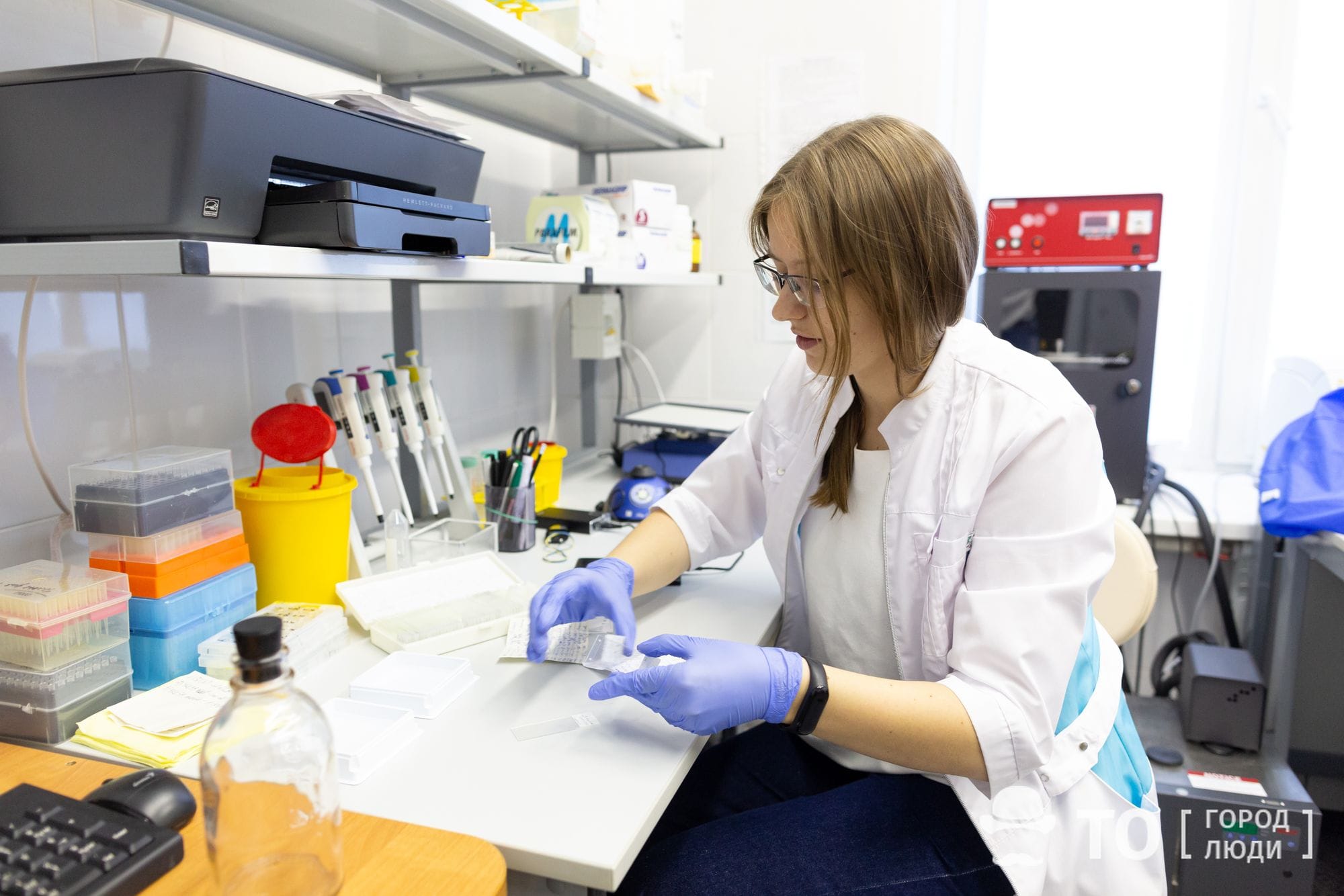
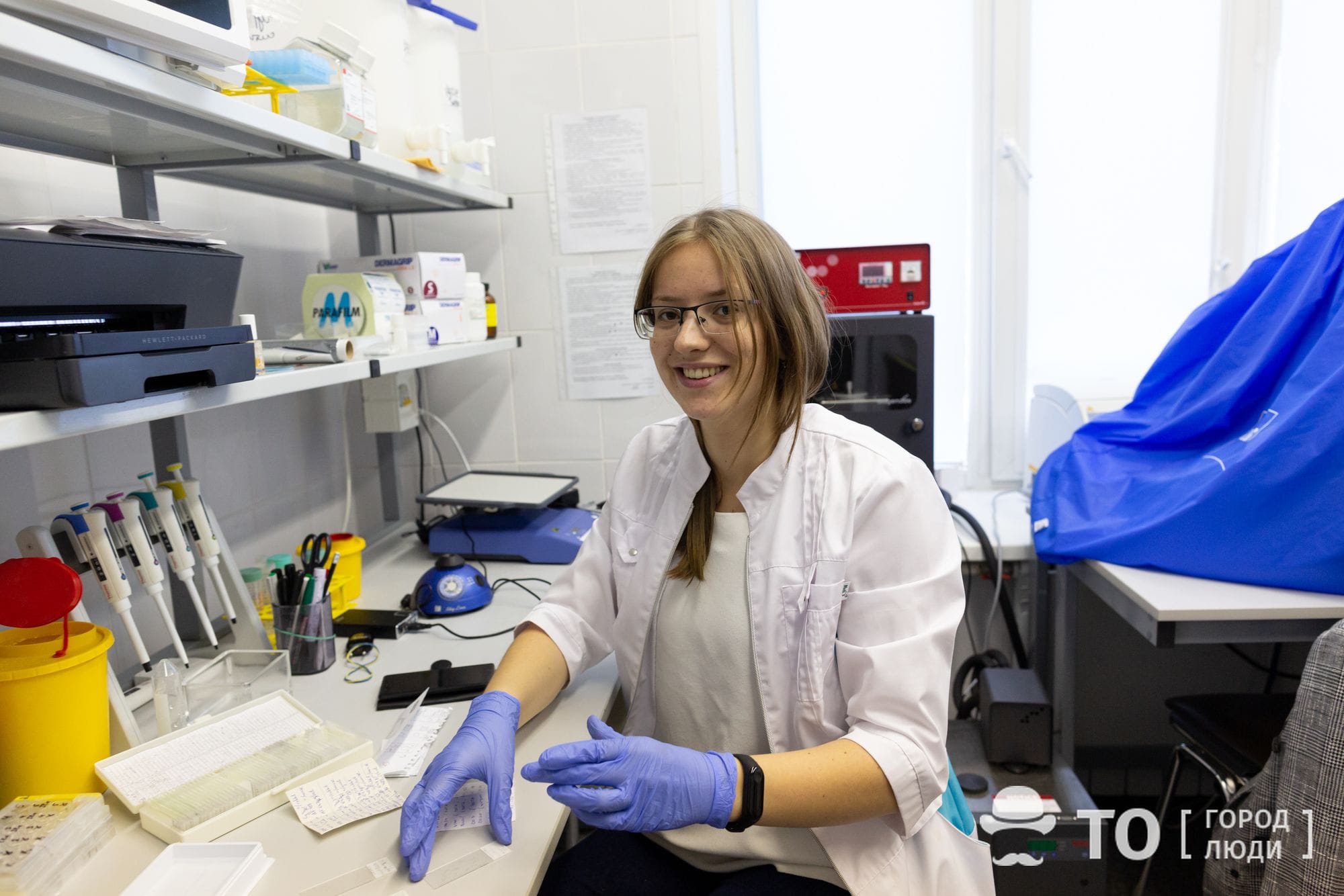
Today we are talking about another laboratory having become part of the Tomsk Center for Biomedicine and Biotechnology. Under the scientific supervision of Julia Kzhyshkowska, Professor, Doctor of Biological Sciences, here biologists and chemists of TSU, doctors and scientists of SSMU [Siberian State Medical University], specialists from Tomsk NIMC [Medical and Research Center] including Oncology Research Institute, Cardiology Research Institute and other scientific institutions of Tomsk, learn to “tame” the key cells of the immune system – macrophages.
The Center for Biomedicine and Biotechnology, being created in Tomsk, will combine the resources of the Tomsk universities of TSU, TPU, TUSUR, as well as NIMC and several research institutes. Inside it, the Collective Use Center, laboratories and educational space will be launched.
Such a project is a new step towards the traditional structures transformation, as a wave of technological innovations gives birth to “greenfield”, a “green field” existing parallel to familiar institutions. This term stands for development of a new space where a new infrastructure is to be created and the opportunity to implement projects from scratch is to be provided. The educational startups growing on this field are named “EdTech” projects.
Cell Changes Its Job

When macrophages, the vanguard of our immune system, begin to respond inappropriately to threats – that it, to ignore dangerous interventions or support internal enemies – this becomes a cause of dangerous diseases, up to oncology and myocardial infarction.
Implant rejection also occurs due to macrophage aggressive behavior. Many diseases, that are deadly now, can be defeated by learning to reprogram these cells and creating materials invulnerable to their “teeth”. This is the basic scientific idea underlying the work of the whole translational cellular and molecular biomedicine laboratory.
By working with the innate immunity cells, our scientific group from the Oncology Research Institute studies the mechanisms of development and treatment resistance of cancers of breast, larynx and stomach. Cardiologists work with cells and tissues of the heart muscle, while chemists and materials scientists develop the implants that would ideally fit the body of each individual patient. But there is a single scientific hypothesis being the cornerstone of all this kinds of research.
In our body, macrophages are present from the very birth, and, if necessary, are formed (differentiated) from specific blood cells – monocytes – throughout our entire life. They are found in all tissues of our body and take care of their daily normal life.
When a dangerous situation arises, macrophages can follow two different paths of development, which are called differentiation and activation. One of these paths provokes an acute immune response allowing you to quickly cope with a bacterial attack and heal a wound, but it can also cause an implant rejection. The other, on the contrary, restrains the immune system and reduces the inflammatory process intensity; but this also can cause health issues, since macrophages may fail to timely respond, for example, to the normal cell transformation into a tumor one, that must be destroyed, and “skip” this situation.
“The ideal result we strive for in the future is to reprogram macrophages, to specify their differentiation and activation paths,” explains Elena Churina, MD, professor of TSU and SSMU, immunologist and allergist, who has been also working on the laboratory project. “By using recombinant cytokines (proteins that regulate the macrophage differentiation) species, we shall be able to achieve the desired effect. Ideally, we shall be capable of introducing this protein directly into the cellular microenvironment or into the cell in the structure of a tumor or inflammation tissue, and specifying the direction of macrophage differentiation we need. But a system for targeted delivery of the species still requires development. This issue is also topical, what we need here is biodegradable polymer materials (microcapsules), the vestiges of which will be removed from the body by the same macrophages, after delivery.”
Fighting Myocardial Infarction and Cancer

Directed macrophage differentiation can help combating many diseases. For example, the recovery process after myocardial infarction also depends on the immune system features. Macrophages begin to operate when damaged cells of the heart muscle become foreign to the body. An inflammatory response is formed, causing cicatrical changes and leading to the cardiac deficiency in the future.
Scientists from the Tomsk Cardiology Research Institute have found that the degree of inflammation and cicatrical changes may not be directly dependent on the area of myocardial damage.
“Our joint research with colleagues from the cardiocenter is unique, since it is conducted on the autopsy material: the hearts of people having deceased from myocardial infarction of varying severity,” explains Elena Churina. “Our employees and graduate students study the cellular composition of the sections of heart muscle, and this allows us to conclude which cells have come there at the time the immune response and the inflammatory process have been developing.
It has been found that sometimes a large area of initial damage is followed by minimal cicatrical changes, and sometimes it is vice versa: an infarction has not been large-focal, but then the cells of the conjunctive tissue that forms the scar, begin to reproduce actively. The heart can no longer effectively perform its pumping function, cardiac deficiency progresses and the person dies. The good news is that these processes can be regulated by decreasing the intensity of the immune response.”
Oncology diseases, that’s another story. Cancer cells can “deceive” macrophages, so instead of killing aggressive tumor cells (that is, forming a protective immune response), the former start helping the latter. In this case, macrophages must be reprogrammed in such a way as to induce maximum activation of the immune response helping the treatment. Cancer immunotherapy is the only hope for success in the fight against tumor cells.
Implants with Personality

Another problem of the modern world is the implant survival rate. People have learned to replace many body parts – from teeth to heart valves – but often the body regards an implant as a foreign element and simply rejects it. Macrophages also take part in this.
“Perhaps, you’ve paid attention that if you do not pull out a splinter, then the inflammatory process will begin, and in the end the splinter will simply dissolve. Macrophages will ‘eat’ it,” says Irina Kurzina, Deputy Head of the Laboratory. “In the same way, the macrophages try to absorb implants. There have been tomographic studies making it possible to literally see the macrophages with hydroxyapatite molecules inside, and this is the material the implants are made of. Moreover, the immune system of each person reacts individually. In one case, the implants survive; in others they cause an acute inflammatory reaction. Everything happens at the cellular level; these mechanisms still need further research.”

As research and clinical practice show, implants made of the same material cause a completely different immune response in the bodies of different patients. There is no material that would universally suit everyone. The chemical composition of the implant appears to be the same, but the immune system reaction to it is unpredictable – it is completely different.
“When some physicists and chemists promise to develop an absolutely tolerogenic material, that is, the one that will cause no immune system reaction at all, unfortunately, they are cunning, as this will never happen,” the immunologist Elena Churina is certain. “Our immune system has evolved in such a way that it recognizes any antigen and responses to it in any case. Our objective is either to modify the material surface, or give it additional properties, in order to minimize the pathological effects of the immune response. These will be tolerogenic materials limiting the occurrence of acute inflammation and implant rejection.”
That is, before introducing the implant into the body, the material must be tested using the macrophage test system consisting of the patient’s own macrophages in order to select an option suitable for the exact patient. This is the very approach to treatment, that is called personalized medicine.
What is on Trend is Transdisciplinarity
As a unit of the university, the laboratory is engaged in teaching students. However, it will keep doing this when in the new Center for Biomedicine and Biotechnology, where the School of Engineering Biology will be created.
At the laboratory and the StrAU [Strategic Autonomous Unit] “Institute of Smart Materials and Technologies”, a unique interdisciplinary Master’s program “Translational Chemical and Biomedical Technologies” has been developed and implemented. In addition to obtaining deep knowledge in various fields of chemistry, the graduate students master the basics of cell biology, general immunology, biochemistry and other biomedical disciplines.
“Now transdisciplinary research is on trend,” says Elena Churina, one of the developers of the Master’s program and a teacher within it. “Specialists working at the intersection of sciences are already highly demanded in the labor market, and in general, I believe that the future lies with them. We are quite pleased with how the Master’s program is implemented. The previous year intake has been 10 students, the one of this year – 11 students, and this is a fairly high indicator, as autonomous Master’s programs often host only 2-3 students. And in the future, of course, we would also like to earn money on this by accepting students on a paid basis.
 The students practice mainly on the basis of partner organizations of the laboratory, that is, in key institutes of Tomsk NIMC [Medical Research Center], primarily in the Oncology Research Institute and the Cardiology Research Institute. There, students have the opportunity to work on unique modern equipment, examine clinical and sectional material, and directly interact with doctors and highly qualified researchers.
The students practice mainly on the basis of partner organizations of the laboratory, that is, in key institutes of Tomsk NIMC [Medical Research Center], primarily in the Oncology Research Institute and the Cardiology Research Institute. There, students have the opportunity to work on unique modern equipment, examine clinical and sectional material, and directly interact with doctors and highly qualified researchers.
The graduates of the two previous classes fulfill themselves in science. Some of them keep working in the laboratory and apply for postgraduate study, some get employed by research institutes, and some leave for other regions and countries.
Advantages of Cooperation

The topic, which scientists in the translational cellular and molecular biomedicine laboratory are engaged in, is so large-scale and complex that it cannot be mastered by a single research team. Obtaining significant scientific results is possible only in collaboration with scientists of various specialties and by combining the instrumental base of several scientific organizations.
The laboratory was initially created in 2014 as a kind of consortium; it hosts not only employees of classical and medical universities, but also scientists from the Tomsk NIMC [Medical Research Center]. These organizations have areas assigned to the laboratory as well; in the Western tradition, such a structure is called the “mirror” one. But strife for cooperation makes the laboratory go further. Since this year, it has also become one of the key laboratories of the Center for Biomedicine and Biotechnology, established in the city of Tomsk.
“Now the world is being structured in such a way that everyone retains his independence, but enters into some alliances,” explains Irina Kurzina. “Previously, the university structure has been kind of feudal: there is a faculty, it includes chairs, laboratories, and all of this obeys the ideology of the dean’s office and academic council. This does not work properly anymore, now organizations and platform structures are quite more open.”
Similar to their colleagues from the TSU Neurobiology Laboratory, the scientists will train students and do scientific work, and, accordingly, use the resources of the Collective Use Center and other scientific organizations being the consortium members.
The equipment necessary for the laboratory work, being already available at the collective use center or planned for purchase, includes, for example, a wider range of DNA sequencing machines. But the main thing is that there will be clean areas with the presence of polluting particles and microorganisms excluded, since now the laboratory areas neither provide, nor allow equipping such a room. To the date, the studies requiring sterile conditions are being implemented on the premises of the Oncology Research Institute.
“This will give us the opportunity to participate in large and serious scientific projects,” Julia Kzhyshkowska and Irina Kurzina answer the question about the advantages of joining the Biomedicine Center. “As a laboratory, we can work on individual issues, but we cannot solve a wide range of problems, because we may lack relevant competencies or instrumental base. And when several laboratories cooperate, this alliance can grant you access to a serious project, financing, and the instrumental base. Together, we get more than we do separately.”